The $100k Mistake: The True Cost of Director of Nursing Turnover
- don2dondevelopment
- 4 hours ago
- 5 min read
Let's talk about the number nobody wants to put on paper.
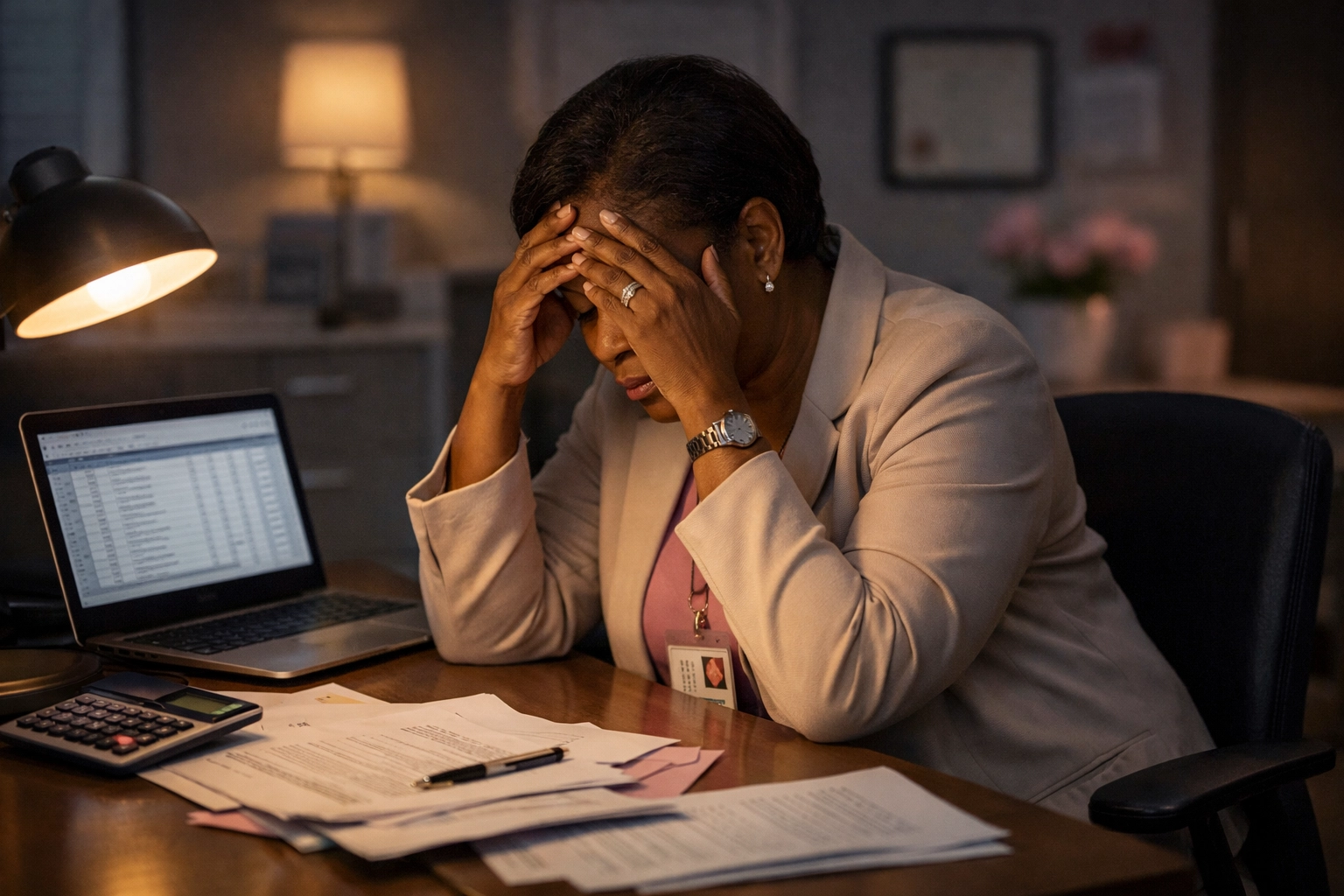
Your Director of Nursing just gave their two-week notice. Or maybe they didn't even give you that courtesy, they just stopped showing up because director of nursing burnout finally won.
Now you're scrambling. You're calling the staffing agency for interim coverage. You're reposting that job listing for the third time this year. And somewhere in the back of your mind, you know this is going to cost you.
But do you know how much?
The real cost of losing a DON isn't just their salary. It's not even close. When you add up recruitment, interim leadership, lost productivity, staff turnover that follows, and the very real risk of survey deficiencies, you're looking at a six-figure hit to your facility.
$100,000. Sometimes more.
And the worst part? It's almost entirely preventable.
Breaking Down the $100k Reality
Let's get specific. Because "turnover is expensive" is something everyone says, but few people actually calculate.
Here's where your money goes when a DON walks out the door:
Recruitment Costs: $15,000–$25,000
Executive-level healthcare recruitment isn't cheap. Whether you're using a headhunter, job boards, or burning through your HR team's time screening candidates, you're spending real money before you even make an offer.
And if your facility has a reputation for burning through DONs? Good luck attracting top talent without sweetening the deal.
Interim Leadership: $30,000–$50,000
You can't run a skilled nursing facility without nursing leadership. So while you're searching for a permanent hire, you're paying premium rates for interim coverage.
Interim DONs are necessary. But at $75–$150 per hour (or more), those weeks add up fast. A 90-day vacancy with interim coverage can easily cost you $40,000 or more, just to keep the lights on.
Lost Productivity and Institutional Knowledge: $20,000+
Your DON knew which CNAs were reliable. They knew which physician got irritable about late callbacks. They knew the surveyor's name and what they always looked for first.
That knowledge walks out the door with them.
The new DON has to rebuild relationships, learn systems, and figure out the unwritten rules of your building. That learning curve costs time. And in healthcare, time is money, and risk.
The Turnover Domino Effect: $15,000–$30,000
Here's the part that really hurts: when a DON leaves, staff follow.
Research shows that when a nurse manager exits, team turnover increases by approximately 2 percentage points in the following year. For DON-level departures, that number climbs higher. Nurses trust their leader. When that leader leaves, especially abruptly, it shakes confidence in the entire building.
Now you're not just replacing a DON. You're replacing the nurses who trusted them.
And with bedside RN turnover costing $40,000–$60,000 per nurse, losing even two or three staff members compounds your losses fast.
Survey Risk and Regulatory Fines: Variable (but Potentially Devastating)
This is the wildcard that keeps Administrators up at night.
A new DON walking into a building with existing deficiencies, or worse, an active Immediate Jeopardy, is a recipe for disaster. Without proper onboarding and stabilization, critical systems fall through the cracks. Care plans get missed. Documentation gaps widen.
And when the surveyor walks in? You're not just paying fines. You're fighting for your facility's reputation.
A single IJ can cost tens of thousands in fines, plus the long-term damage to your star rating and census.
The Hidden Cost Nobody Talks About
The spreadsheet tells one story. But there's another cost that doesn't show up in your P&L statement.
Morale.
When your building churns through DONs, your staff notices. They start whispering. They start updating their own resumes. The phrase "here we go again" becomes the unofficial motto.
Staff retention in nursing homes is directly tied to leadership stability. When the person at the top keeps changing, frontline workers feel abandoned. They lose faith that things will ever get better.
And that feeling? It spreads faster than any policy memo you could send.

Why Does This Keep Happening?
Here's the uncomfortable truth: most facilities set their DONs up to fail from Day One.
Think about the typical onboarding experience for a new Director of Nursing:
Day 1: Here are your keys. Here's the EMR login. Good luck.
Week 1: Active IJ on the desk. Half the nursing schedule is open. No one tells you where the supplies are.
Month 1: You're expected to fix everything the last DON couldn't fix, with no context, no support, and no backup.
This is the "sink or swim" culture that has become normalized in nursing home leadership.
We take our best clinical minds, promote them into impossible situations, and then act surprised when they burn out or quit.
Director of nursing burnout isn't a character flaw. It's a systems failure.
And every time it happens, you write another $100,000 check.
The 90-Day Investment That Changes Everything
What if instead of crossing your fingers and hoping your new hire survives, you actually invested in their success?
That's where a structured 90-day onboarding and stabilization program comes in.
Here's what real support looks like:
Phase 1: The Deep Dive (Days 1–30)
Before your new DON drowns in daily fires, they need to understand what they're walking into. A stabilization partner audits your clinical systems, identifies the gaps, and creates a roadmap, not a to-do list that makes them want to quit.
Phase 2: Plugging the Holes (Days 31–60)
This is where the real work happens. Side-by-side mentorship. Building systems that prevent problems instead of just reacting to them. Addressing staffing patterns, documentation workflows, and the cultural issues that previous leaders couldn't fix alone.

Phase 3: Sustainable Leadership (Days 61–90)
By the end of 90 days, your DON isn't just surviving, they're leading. They have the confidence, the systems, and the organizational support to stay for the long haul.
The cost of a 90-day stabilization program is a fraction of the $100k you'll spend replacing another DON.
It's not an expense. It's insurance.
The Math That Should Keep You Up at Night
Let's say you're an Administrator who has replaced your DON twice in the past 18 months.
That's $200,000 gone. Maybe more.
Now imagine you had invested $15,000–$25,000 in a proper onboarding and stabilization program for that first hire. Imagine they had real support, not a binder and a prayer.
Would they still be there?
The answer, more often than not, is yes.
Staff retention in nursing homes starts at the top. When your nursing leadership is stable, your building is stable. When your building is stable, your staff stays. When your staff stays, your residents get better care.
It's not complicated. It's just rarely prioritized.
A Different Approach to Nursing Home Leadership
The industry has accepted the revolving door in the DON office as inevitable. It's not.
What's inevitable is the outcome when you keep doing the same thing: hire, abandon, lose, repeat.
The facilities that break this cycle are the ones willing to invest in their leaders before they break. They're the ones who recognize that a great DON doesn't need to quit just to survive.
If your building is stuck in the turnover loop, it's worth asking: what would it cost to actually support your next hire?
And what has it already cost you not to?
The $100k mistake isn't the cost of a bad hire. It's the cost of a good hire who never got the support they needed to succeed.
Comments