The Invisible Burnout: For the DON Who Refuses to Quit but Can't Keep Floating
- don2dondevelopment
- 4 hours ago
- 5 min read
You're not going to quit.
I already know that about you. You've been in this building for a year: maybe longer. You know every resident by name. You know that Mrs. Patterson likes her coffee with two sugars and that Mr. Williams only calms down when Keisha is on shift. You know your CNAs are exhausted, but they show up for you because you've never asked them to do anything you wouldn't do yourself.
You love these people. That's why you're still here.
But here's what I also know: you're drowning. And nobody sees it.
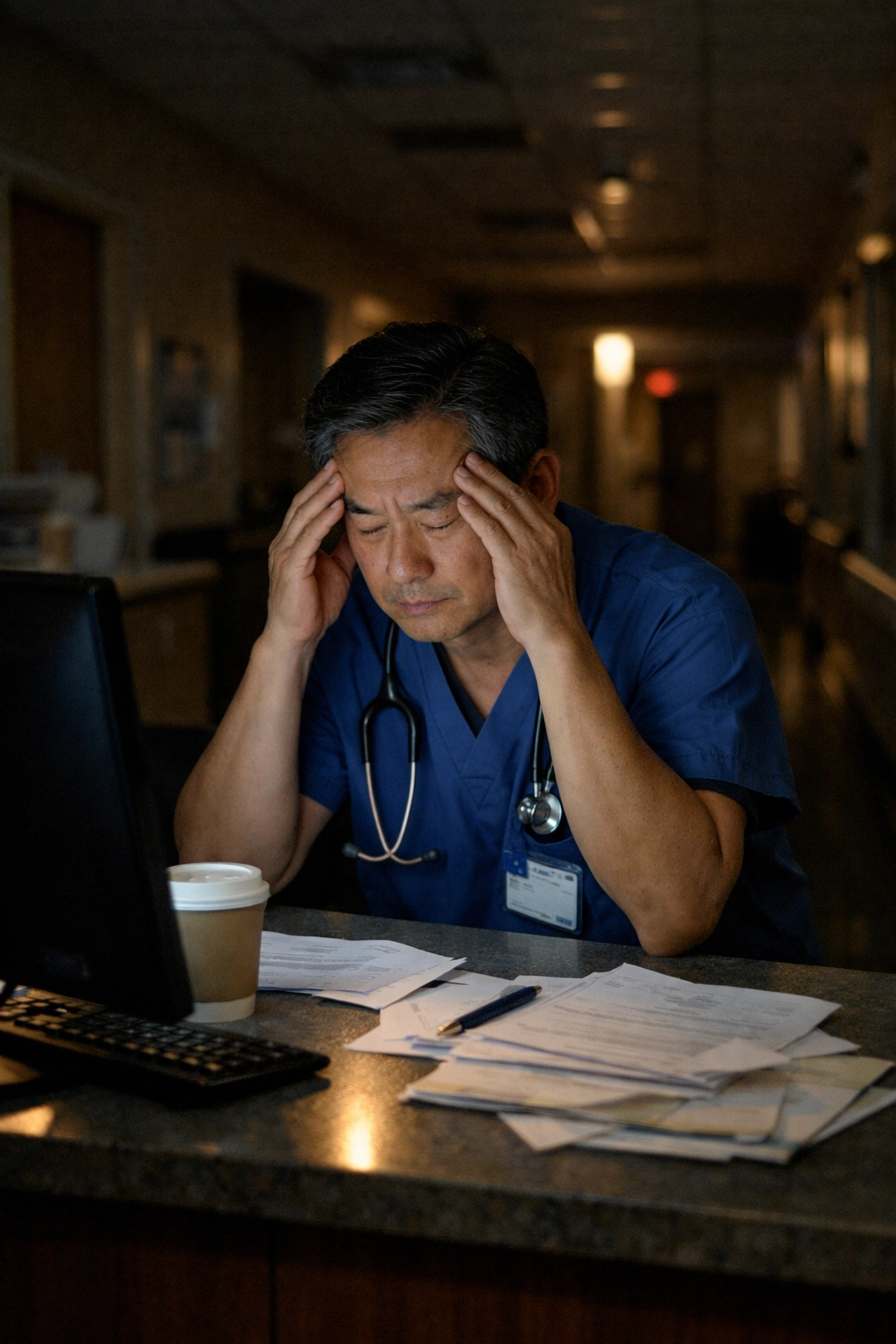
The Kind of Burnout Nobody Talks About
When people talk about director of nursing burnout, they usually picture someone slamming their badge on the desk and walking out. They picture the dramatic exit, the resignation letter, the "I've had enough" moment.
But that's not you.
Your burnout is quieter. It's the kind where you sit in your car for ten extra minutes before walking in, just trying to gather yourself. It's the Sunday night dread that starts on Saturday afternoon. It's the way you've stopped eating lunch because there's always one more fire to put out.
You're not quitting. But you're also not okay.
This is invisible burnout: and it's the most dangerous kind because everyone assumes you're fine. You're still showing up. You're still fixing problems. You're still holding the building together with duct tape and sheer willpower.
But inside? You're running on fumes, and the tank has been empty for months.

You've Asked for Help. Nobody Listened.
Here's the part that makes invisible burnout so painful: it's not like you haven't tried.
You've gone to your Administrator. You've explained that you need more support: maybe another nurse on the floor, maybe help with the mountains of paperwork, maybe just someone to listen without immediately pivoting to budget concerns.
And what happened?
Maybe you got a sympathetic nod and a "we'll see what we can do" that turned into nothing. Maybe you got a lecture about doing more with less. Maybe: and this one stings the most: they actually sent "help."
But it wasn't the help you needed.
It was a consultant with a clipboard. Someone from corporate who walked the halls for two days, pointed out everything you were already painfully aware of, and left you with a 47-page report that somehow became your responsibility to implement. On top of everything else.
That's not support. That's more weight on shoulders that are already breaking.
The Emotional Math That Keeps You Stuck
Let's be honest about why you haven't left.
It's not the paycheck: you could probably make more money somewhere else with less stress. It's not the title. It's not even the benefits.
It's the people.
You think about what would happen to your team if you walked away. Maria, who's been with you since day one and finally started believing in herself as a charge nurse. Devon, who drives 45 minutes each way because he says this is the only building where leadership actually cares. The new grad you've been mentoring who reminds you of yourself fifteen years ago.
And the residents. God, the residents.
You know that Mr. Chen's daughter only trusts you with updates about her father. You know that half of your dementia unit responds better to familiar faces, and a leadership change would set them back months. You know that in long-term care, continuity matters more than almost anything else.
So you stay. You keep floating. You tell yourself you'll figure it out.
But here's the math that's killing you: you cannot pour from an empty cup, and you cannot stabilize a building while you're destabilizing yourself.

The "1.2 Problem" Nobody Warned You About
Research calls it the "1.2-FTE problem": healthcare leaders are consistently expected to complete 1.2 full-time equivalents of work. That extra 20% is invisible on any balance sheet, but it's the defining struggle for nursing leadership in long-term care.
It shows up in the charting you do at 10 PM from your kitchen table. It shows up in the texts you answer on your day off. It shows up in the emotional labor of holding space for your staff's trauma while processing your own.
And here's what makes it worse: the care work you do: the real, human, relationship-building work that actually makes your building run: doesn't fit neatly into any metric. It's invisible. It's not valued by the systems that evaluate your performance.
So you're doing 120% of an already impossible job, and 40% of that work doesn't even "count."
No wonder you're drowning.
What Actual Support Looks Like
I want to tell you something important: you are not failing. The system is failing you.
But I also want to tell you this: there is another way.
Real support for a director of nursing doesn't look like a consultant with a clipboard. It doesn't look like another webinar on "self-care" or a pizza party for Nurses Week. It doesn't look like being told to "delegate more" when there's no one to delegate to.
Real support looks like someone who has actually stood in your shoes: someone who knows what it's like to walk into a building with an IJ on the desk and half the schedule open. Someone who understands that leadership in long-term care isn't about spreadsheets; it's about people.
Real support means having a partner who can help you stabilize your clinical systems so you're not constantly in crisis mode. It means building a team that can function without you holding every single piece together. It means creating breathing room so you can actually lead instead of just survive.
You Deserve More Than Survival Mode
I want you to imagine something for a minute.
Imagine walking into your building and not immediately bracing for impact. Imagine having systems in place that catch problems before they become fires. Imagine a team that's trained, supported, and stable enough that you can take a sick day without the whole thing falling apart.
Imagine feeling like a leader again instead of a lifeguard.
That's not a fantasy. That's what happens when you get the right support: not corporate band-aids, but real, in-the-trenches partnership from someone who gets it.
This Is Your Permission Slip
If you've read this far, I want you to hear me clearly:
Asking for help is not weakness. Staying silent while you drown is not loyalty. And loving your residents doesn't mean you have to sacrifice yourself.
You've been fighting alone for too long. You've been holding it together with nothing but heart and hustle, and while that's admirable, it's not sustainable. The residents you love deserve a DON who isn't running on empty. Your staff deserves a leader who has enough left to actually lead.
And you? You deserve to remember why you became a nurse in the first place.
At Don 2 Don Development, we don't show up with clipboards and criticism. We show up with experience, empathy, and a 90-day plan to stabilize your building so you can stop drowning and start leading.
Because a great DON shouldn't have to choose between the job she loves and her own well-being.
You've been floating alone long enough. It's time to grab the lifeline.
Comments